Blogs & News
Empowering Recovery: OrthoCarolina's Multidisciplinary Approach to Brachial Plexus Injuries, Limb Paralysis, and Congenital Hand Differences
Discover how OrthoCarolina's multidisciplinary approach provides comprehensive care for brachial plexus injuries, limb paralysis, and congenital hand differences. From innovative treatments to personalized rehabilitation, we're committed to enhancing physical, emotional, and psychological well-being.
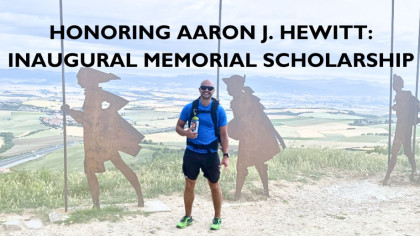
Read MoreHonoring Aaron J. Hewitt: Inaugural Memorial Scholarship
Discover the legacy of Aaron J. Hewitt with the inaugural memorial scholarship awarded to Scot Rheinecker, PA-C at OrthoCarolina. Celebrate excellence, leadership, and compassion within our community.
Read MoreEric Hunt's Remarkable Comeback: From Quadricep Tendon Rupture to Powerlifting
Discover Eric Hunt's awe-inspiring journey from a ruptured quadricep tendon to powerlifting glory. Follow his resilience, rehabilitation, and ambitious comeback goals after overcoming adversity. A tale of strength, determination, and the unwavering spirit that defines extraordinary comebacks.
Read MoreSwinging Through Adversity: William Busse's Journey to Relief and Resilience with Knee Injections
Discover William Busse's inspiring journey from knee pain to resilience with the help of knee injections, offering hope and relief in the face of adversity.
Read MoreExploring Targeted Muscle Reinnervation: Hands in Motion Podcast with Dr. Bryan Loeffler & the ASHT
Dive into the world of targeted muscle reinnervation with Dr. Bryan Loeffler on the Hands in Motion podcast, hosted by Cara Smith, PT, DPT, CHT, and Stephanie Strouse, OTD, OTR/L, CHT. Gain insights and expert knowledge in this engaging discussion.
Read MoreLet OrthoCarolina Assist You When Conquering Shin Splints
Learn effective strategies for managing shin splints in soccer players and runners. Discover expert advice for pain management, injury prevention, and staying in the game pain-free.
Read MoreDancing Through Adversity: Kelsey Ormiston's Resilient Return to the Stage with OrthoCarolina
Join Kelsey Ormiston's remarkable journey back to dance after kneecap dislocations with OrthoCarolina's, Dr. Riboh, who helped Kelsey return to dance.
Read MoreGreen Thumb, Healthy Joints: Gardening Tips for Orthopedic Wellness
Elevate orthopedic wellness with our Green Thumb Gardening Tips – your guide to cultivating healthy joints through joint-friendly techniques. Explore expert advice, sustainable garden care, and horticultural insights for a vibrant garden and a healthier you.
Read MoreScrape the Pain Away: The Graston Technique®
Modeled from the centuries-old Chinese Gua Sha technique, the Graston Technique® relies on a special stainless-steel tool and massage method to stimulate blood flow and promote healing.
OrthoCarolina Receives The Triple Crown in Research Awards: Advancing Orthopedic Care Through Groundbreaking Research
Explore OrthoCarolina's groundbreaking research, winning top awards from AAOS and AAHKS. Discover how our innovative studies are transforming orthopedic care, from revolutionizing treatment protocols for prosthetic joint infections to advancing opioid-free pain management in spine surgery.
Read MorePediatric Scoliosis Webinar Recap: Navigating Pediatric Scoliosis: Understanding, Treatment, and Long-Term Care
Explore scoliosis types, treatments, and diagnostics, including the Cobb angle and various scoliosis forms. Learn about bracing, surgery, and effective management through physical therapy. Gain insights into adolescent concerns, addressing back pain, muscle imbalance, and post-surgery care.
Read MoreNavigating the Winter Court: Safeguarding Your Steps in Cold-Weather Pickleball
Stay injury-free on the winter pickleball court with our expert tips! Explore strategies for cold-weather play, discover essential foot and ankle injury prevention techniques, and find the best pickleball footwear. Enhance your safety and enjoyment with specialized warm-up exercises and Achilles injury prevention. Master the art of winter pickleball with our comprehensive guide
Read MoreA Journey to Recovery: Emily's Triumph Over Shoulder Injury
Follow Emily's inspiring journey of overcoming shoulder pain with OrthoCarolina. Discover how Dr. Grant Mostak's expertise and cutting-edge treatment led to a successful recovery, allowing Emily to return to championship-level beach volleyball after a SLAP tear surgery.
Read MoreCelebrating Women Physicians at OrthoCarolina Through Women Physician Month
Explore the groundbreaking contributions of Women Physicians at OrthoCarolina throughout February. Celebrating diversity in the orthopedic field, discover the expertise and dedication of these trailblazing specialists, shaping a future of medical empowerment.
Read MoreHow to Create Your Own Winter X Games Safely: Navigating Extreme Thrills with Expert Insights
Unlocking the Secrets to Injury Prevention and Optimal Performance in High-Stakes Winter Sports.
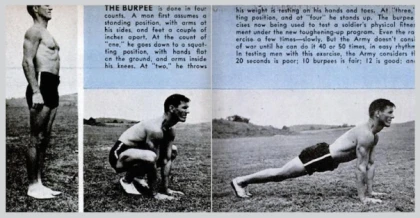
Read MoreRoyal H. Burpee Was a Real Person: Beyond the Name, the Man Behind the Iconic Fitness Test
From CrossFit to functional training, discover how burpees offer a dynamic combination of aerobic and strength exercises for a fun and effective workout experience.
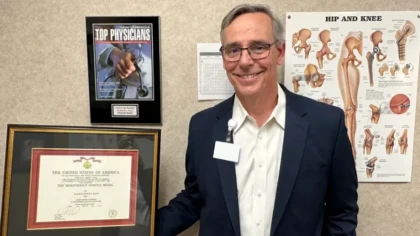
Read More50 OrthoCarolina Doctors Named Top Docs!
Discover the 50 distinguished OrthoCarolina Physicians who have achieved the esteemed 'Top Docs' recognition in Charlotte. These dedicated medical professionals have been honored based on a peer survey conducted by Castle Connolly and are at the forefront of healthcare excellence in the region
Read MoreStride into Wellness: Navigating the Path of Joint Health and Fitness – Exploring the Harmony of Walking and Running
Explore the world of optimal joint health and fitness with expert orthopedic insights. Discover the benefits of walking and running, strike a balance for overall fitness, and delve into effective weight management strategies tailored for women.
Read MoreOC Presents the 2024 Sports Medicine Symposium
The 36th Annual Sports Medicine Symposium, presented by OrthoCarolina, will be held on Saturday, February 10, 2024, at the Dale F. Halton Theater.
Read MoreWelcome Dr. Aversano!
Discover the expertise of Michael W. Aversano, MD, a distinguished Pediatric Hand Specialist at OrthoCarolina. Explore his extensive background, publications, presentations, and contributions to the field of orthopedic surgery.
Read MoreNavigating the holiday hustle and bustle with Orthopedic conditions
Discover practical tips for navigating the holiday season with orthopedic conditions. Prioritize self-care, use ergonomic tools, and manage pain effectively. Stay active and stress-free while embracing the festive spirit
Read MoreOrthoCarolina: Unparalleled Expertise in Orthopedics
Discover OrthoCarolina: Your trusted source for specialized orthopedic care. Our expert orthopedic surgeons provide personalized solutions, unmatched expertise, and state-of-the-art facilities.
Read MoreOC Foot & Ankle's 15-Year Commitment: 'Our Hearts to Your Soles' - Bringing Comfort, One Step at a Time
Our Hearts to Your Soles' program. Join OC Foot & Ankle as they distribute over 150 pairs of shoes, generously donated by Red Wing Shoes, making a lasting impact on the lives of the less fortunate in Charlotte. Explore the roots of compassion that started in 2004 and witness the evolution of a legacy dedicated to providing proper footwear and medical foot screenings to those in need.
Read MoreFrom Military Service to Surgical Excellence: The Inspiring Journey of Dr. Pat Hayes
Discover the inspiring journey of Dr. Pat Hayes, a veteran and orthopedic surgeon, whose beginnings in a military family led to a remarkable career. From making a lasting impact on his community and beyond, explore the transformative power of military service and the legacy of service that inspires others. Join us in honoring Dr. Hayes's story on Veterans Day and celebrating the resilience, dedication, and generosity that define his extraordinary life.
Read MoreResilience and Return: Eli Patrick's Clavicle Fracture and the Journey Back to Adventure
Join Eli Patrick on his remarkable journey from a snowboarding mishap and clavicle fracture to a successful orthopedic surgery by Dr. Burbank. Discover how he overcame the challenges, battled post-surgery physical therapy, and returned to his beloved adventure sports with unwavering determination. Follow Eli's story of resilience, and find inspiration in his fearless pursuit of high-risk activities.
Read More